A rush transcript of the Governor's remarks is available below:
Good morning. Happy Sunday. For those of you who celebrate Happy Palm Sunday. Happy Passover week for those who celebrate Passover. Thanks for taking the time to be with us today. We want to give you an update as to where we are.
The number of cases increase which is nothing new. It's happened every day since we've started this. It's been a long month. Something a little bit different in the data today. We're not really 100 percent sure yet what the significance is as we're feeling our way through this.
Number of people tested, 18,000. Positive cases are up 8,000, total of 122,000 cases. Number of patients discharged, total discharged is 12,000 - 1,700 discharged in one day. Number of deaths is up. That's the bad news. It's 44,159 and we pray for each for each and every one of them and their families and that is up and that is the worst news.
But the number of deaths over the past few days has been dropping for the first time. What is the significance of that? It's too early to tell. This is the impact by state. But as I said the interesting blip maybe in the data, or hopeful beginning of a shift in the data and the number of cases, total number of new hospitalizations is 574 which is obviously much lower than previous numbers. That's partially a function of more people being discharged but you see ICU admissions are also down. The daily intubations down slightly from where it was. Again, you can't do this day to day. You have to look at three or four days to see a pattern.
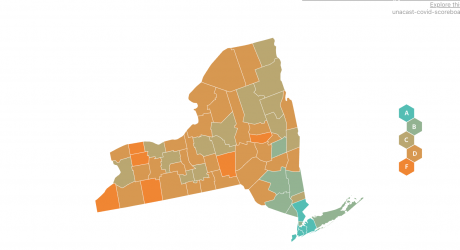
Discharge rate is way up and that's great news and the statewide balance of cases has been relatively stable for the past few days. There is a shift to Long Island. Upstate New York is basically flat and as Long Island grows the percentage of cases in New York City has reduced.
For those people who look at the data, you have all these projection models and what's been infuriating to me is the models are so different that it's very hard to plan when these models shift all the time. But there's also a difference of opinion on what happens at the apex. All the models say you go up until you go down - thank you very much. Then there's a difference of, is the apex a point or is the apex a plateau. In other words you go up, hit the high and the immediately drop, or do you go up and then there's a plateau where the number of cases stays high for a period of time and then drops? There's a difference of opinion.
So you have to think about that when you think about what you're seeing in the numbers because you could argue that you're seeing a slight plateauing in the data which obviously would be good news because it means you plateau for a period of time and then you start to come down and we're all feeling our way through this and we have the best minds in the country, literally on the globe, advising us because New York is the first. I also think it will be very helpful for the other states that follow. I was just talking to Dr. Zucker about codifying everything we're learning because when the next states start to go through this we hope that they can benefit from what we're going through.
But we're looking at this seriously now because by the data we could be either very near the apex or the apex could be a plateau and we could be on that plateau right now. We won't know until you see the next few days. Does it go up, does it go down, but that's what the statisticians will tell you today.
As we've said before, the coronavirus is truly vicious and effective at what the virus does. It's an effective killer. People who are very vulnerable must stay isolated and protected. I mean, that was the point from day one. That was the point with Matilda's Law, my mother. You have to isolate and protect those people. If a very vulnerable person gets infected with this virus, the probability of a quote unquote "cure" is very low. And that's what this has really been about from day one. That small percentage of the population that's very vulnerable. Major effort that has impacted everyone to save the lives of those people who are in the very vulnerable population. If you're not part of that vulnerable population, then you will get sick, 20 percent require hospitalization, but the hospital system is very effective and it makes a real difference. And that's why the highest number of people ever now being discharged, right.
So you're just seeing the evolution of this whole story. You're seeing the narrative unfold, right. We're all watching a movie, we're waiting to see what the next scene is, and as the movie unfolds you start to understand the story better and better. Rush of infection rate, rush of people into the hospital system, hospital system capacity explodes, more people are in, but, more people are coming out. 75 percent of those people who have now gone into the hospital system are coming out of the hospital system. It also helps with the capacity of the hospital system because obviously the more people who are coming out, it makes it easier to handle the large influx that's coming in.
Having said all of that, the operational challenge for the healthcare system is impossible. Because the system is over capacity, all across the board. It's just over capacity. So what we're basically saying to a system is you have to manage with the same resources that you have, same staff, an over-capacity situation. And that is putting a tremendous amount of stress on the healthcare system. You're asking a system to do more than it has ever done before, more than it was designed to do with less. I understand that. I get that. Day in and day out, the commissioner and everyone at this table deals with the healthcare system. I understand what they're dealing with. I understand they're being asked to do the impossible. And they are being asked to do the impossible. But, life is options and we do not have any other options. So you get to a situation and you do what you have to do in that situation. And that's where we are. The only operational plan that can work, right, because you know the system doesn't have the capacity, doesn't have the supplies, doesn't have the staff. So how do you handle this surge over capacity?
We call it, we have to surge and flex, which means you have to deal with, if you're an individual hospital or hospital network, yes, you're going to be over capacity. And the only way we can make this work is if we flex the system so that we take all hospitals, all hospital networks, some hospitals are in networks, and we work together as one system, which has never been done, right. We have public hospitals. We have private hospitals. We have Long Island hospitals. We have New York City hospitals. In totality, it's the health care system, the state manages, regulates the healthcare system, but they're all individual hospitals. And, or individual networks. And they are accustomed to just doing business and managing their own affairs. That doesn't work. We have to balance the patient load among all of these hospitals. So if one hospital starts to get high or has a protected high intake, we have to shift that patient load to other hospitals. That means some patients who show up at their neighborhood hospital may be asked, can we transport you to another hospital, which is not in your neighborhood, but actually has more capacity. So we have to adjust that patient load among all of the hospitals, which is a daily exercise and it's very, very difficult.
We're running short on supplies all across the board. Some hospitals happen to have a greater supply of one thing or another. One hospital has a greater supply of masks, one hospital has a greater supply of gowns. And when we're talking about supply, hospitals are accustomed to dealing with a 60-day supply, 90-day supply. We're talking about 2 or 3 or 4 day supply, which makes the entire hospital system uncomfortable, which I also understand because we're literally going day-to-day with our supplies, with out staff, et cetera. Which is counter-intuitive and counter-operational for the entire health care system and I understand that also.
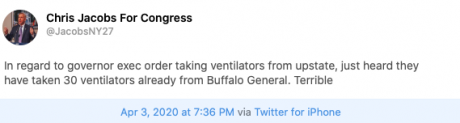
The big operational shift will be Javits coming online if we get that up and running efficiently. That's 2,500 beds for people who test positive with the COVID virus. That is a major shift for the systems and at a time when we desperately need a relief valve for the system, Javits could do that. We're working very hard to get that up and running. That rolling deployment, that flexibility - there is no other way to do this on the state level. I can't say to a hospital, I will send you all the supplies you need. I will send you all the ventilators you need. We don't have it. We don't have them. It's not an exercise, it's not a drill. It's just a statement of reality. You're going to have to shift and deploy resources to different locations based on the need of that location. I think that's going to be true for the country. The federal government everyone says federal stockpile, federal stockpile. There's not enough in the federal stockpile to take care of New York and Illinois and Texas and Florida and California. It's not an option. The only option I see is there's a national deployment - everyone says this is wartime, it is a war and the virus is the enemy - where help New York today, thank you state of Oregon, we're dealing with this curve today and this intensity and then nationally, we shift the resources to the next place that is most impacted.
Just what we're doing in New York City and New York State on a microcosm, we shift resources from the Bronx to Brooklyn to Queens to Nassau. Shift national resources and state resources from New York to Florida to Illinois, whatever is next on the curve. We're going to do that in any event. We get through this, people have been so beautiful to us and it is the New York way. We're going to codify everything we've learned and when we get past this curve, whatever part of the country goes next, we will be there with equipment and personnel and however we can help.
Federal government is also deploying approximately 1,000 personnel to New York. That's doctors, that's nurses, that's respiratory technicians. The immediate priority is to deploy those people to help the New York City public hospitals. The New York City public hospital system, H&H, was a system that was under stress to begin with before any of this. So obviously, you add more stress to institutions that were under stress, it only makes the situation more difficult so we're going to deploy all the federal personnel who are coming in today, 325, to the New York City public hospital system.
I talk to the hospital administrators on a daily basis. We get them on a conference call and we do this shifting of supplies and balancing of patient load. I know that I'm asking them to do really difficult things, I get it. I don't enjoy being in this situation. I don't enjoy putting them in this position. I know their staff is all over burdened, but all I can say is thank you to the administration of this health care system and most importantly thank you to the frontline workers. These people, they are true heroes in the truest sense of the word, what they do day in and day out under very difficult circumstances, and we thank them all.
On a different and somewhat lighter note, there is an accompanying affliction to the coronavirus that we talked about early on. It is cabin fever. It is a real situation. Not medically diagnosed, I asked Dr. Zucker there is no medical diagnosis for cabin fever, but I believe it exists. It is a feeling of isolation. It is often accompanied by radical mood swings, resentment of people around you to varying degrees, for no reason whatsoever. Just an upwelling of resentment, especially toward people who are in apparent positions of authority in this situation which I've noticed. Irrational outbursts can come at any time, without any warning. Just an irrational outburst, frustration, anger, with no rational basis. Cabin fever, in many ways, also threatens the essence of our Constitution, which is premised on people sharing domestic tranquility and it can be disruptive to tranquility. I can attest to that. It is a real thing. Think about it. It has only been one month but it has been a long month.
Positive intervention for cabin fever, I am going to take up running again. I used to run in the normal days before this job. But I am going to start running again. My daughter Cara, we will run as a family and go out there. Cara has a head start. She is out there doing five miles every day. She thinks she can beat me. Give me a couple of weeks and I will be right there, right there. Fast like lightning. We are going to do it. We will make the dog come. The dog is also experiencing cabin fever. He's a little disrupted. The order of the pack has changed. Different people, he does not know where he fits. He has anxiety. He is going to run. Think of ways to deal with it. I don't have any great answer.
But a little perspective on the whole situation is important. I challenged my daughters, this is terrible, this is terrible, this is terrible. I have been saying this is terrible for society, the economy and personally. But, you know, let's look back at history, right? Generations have gone through terrible times. So, my challenge to them is you find me a generation that has had a better overall situation than where we are right now. Go back to World War I, World War II, Vietnam, 1918 flu pandemic, you find me a generation that has not had a challenge to deal with and we will are going to have that discussion. Keep in mind on perspective. This is going to be over. You can see the story developing. You can start to see how the story ends, right? They will have a vaccine. Will it be 12 months or 14 months or 18 months? There are a number of treatments that are being expedited and are being tested right now. Dr. Zucker of New York is working expeditiously and cooperatively with the FDA to try all new different treatments: convalescent plasma, receptor antibody treatments, we are working on the hydroxychloroquine - we are working on it aggressively. So, we are trying all these new treatments. Some of them show real promise. But, you can see where the story ends.
I think, this is opinion and not fact, I think you see the return to normalcy when we have an approved rapid testing program that can be brought to scale. We are now testing rapid testing programs. But, when you get to the point where you can do rapid testing, of scale, and people can start to go back to work because they know they are negative. We continue to protect the vulnerable population, which is what this was about, and we liberate, as my daughters would say they are seeking liberation. We liberate people who can go back to work because we know that they are not in the vulnerable category and they are negative. I think that is, it is under development now, the rapid testing, and we are part of it. That is going to be the answer, I believe. And we get through it because we are New York State tough. Thank you.